Tabitha Mwangi, Pwani University
Myths about diseases spread like wildfire. Malaria is a case in point. The Conversation Africa’s Health and Medicine Editor Joy Wanja Muraya asked Tabitha Mwangi to help sort out fact from fiction. ![]()
Mosquitoes only bite at night.
Not entirely true.
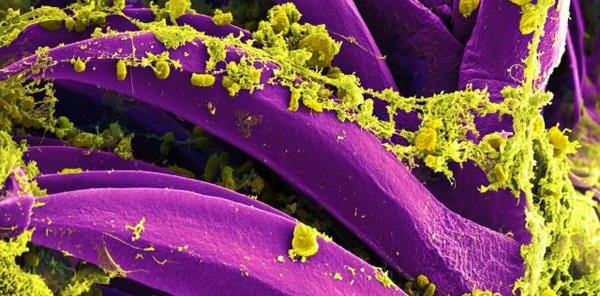
There are two types of mosquitoes that bite mostly at night; the Anopheles mosquito that transmits malaria and it’s noisier cousin, the Culex mosquito which spreads lymphatic filariasis, – also known as elephantiasis – that presents as severe swelling in the arms, legs or genitals.
A year-long study in Western Kenya showed that 15% of the mosquitoes bite between 6pm to 9pm while the majority (85%) bite from 9pm till morning. Data from this study puts further emphasis on the value of sleeping under an insecticide treated bednet.
But there are other mosquitoes, such as the Aedes mosquitoes – easily identified by their zebra stripped legs – that are active mostly during the day. They spread viruses that cause dengue, zika, Chikugunya and rift valley fever.
The fact that this mosquito is active during the day makes it harder to control the diseases it spreads because bed nets aren’t an option.
Eating garlic before I sleep will repel mosquitoes.
There’s no scientific evidence to support this.
Garlic does produce a sulphur compound known as allicin which has some anti-bacterial, anti-fungal and anti-parasitic activities. Researchers have looked at it’s impact on mice that have been infected with malaria. In mice, use of allicin leads to a reduction in the number of malaria parasites in the blood, the higher the dose of allicin, the longer the mice survived. But no research has been done on its effect on the human immune system.
Garlic oils are marketed as insect repellents but their efficacy is uncertain.
Mosquitoes like to bite women and children more than men.
This isn’t true, though there’s some evidence that they’re partial to pregnant women.
In The Gambia researchers found that pregnant women are twice as attractive to mosquitoes than non pregnant women.
The research involved 36 pregnant women and 36 women who weren’t pregnant. The two groups slept in separate huts under bed nets. In the morning, researchers collected and counted the mosquitoes found in the separate huts.
Twice as many mosquitoes were found in the huts in which the pregnant women had slept. There were two possible explanations for this. The first is that mosquitoes are attracted to carbon dioxide which pregnant women produce more of. In advanced pregnancy, women exhale 21% greater volumes than non pregnant women.
The second possible explanation is that pregnant women’s tummies are 0.7°C warmer than non pregnant women which could attract mosquitoes.
But there was an additional factor that the researchers suggested could have affected the results. Pregnant women – particularly women in advanced pregnancy – had to leave their huts at night more often than non-pregnant women because they need to urinate frequently.
Mosquitoes die after feeding.
This is not true. Male mosquitoes feed on sugary things while female mosquitoes need blood for their eggs to develop.
After feeding on blood, a female mosquito will rest to digest the blood and wait for the eggs to be ready.
The female mosquito rests for about two to three days then lays her eggs in water. After laying between 50 to 200 eggs, she then searches for another blood meal in order to lay another batch of eggs.
During her lifetime the female tries to lay as many eggs as she can which requires several blood meals.
In a laboratory, female mosquitoes can live for up to one month. But in natural conditions, few survive beyond one to two weeks.
Once you get malaria, you will never get it again.
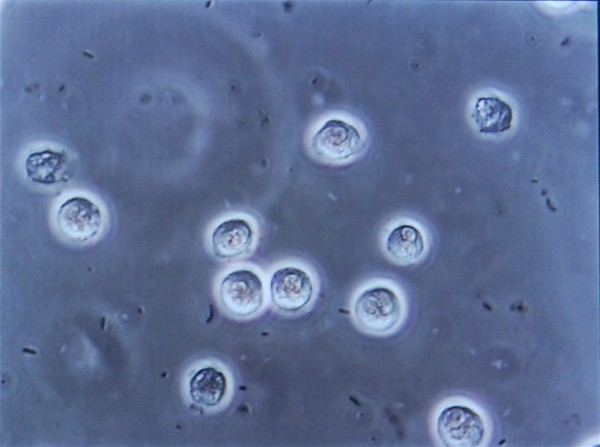
Researchers have spent years monitoring people in malaria endemic areas to learn the patterns of immunity.
My PhD research involved collecting data on malaria from about 1,000 people in Coastal Kenya for two years. Children under five years had, on average, one clinical attack of malaria every year.
Malaria cases declined steeply after that and it was rare for adults who lived in this malaria endemic areas to have clinical attacks.
Other studies have shown that when highly immune adults spent long periods of time in places where they weren’t being bitten by infected mosquitoes, they could lose some of thatimmunity.
Scientists know that solid immunity to malaria only occurs in people who are constantly challenged. But it’s still not clear how this happens. This is one of the reasons why developing a malaria vaccine that works well has proved so difficult.
Mosquitoes only like the blood of humans.
This is true for some mosquitoes, but because female mosquitoes need a blood meal, most will take it from wherever they can find it. For example, livestock kept outside the homestead can attract mosquitoes. There’s even been a suggestion that cattle should be treated with insecticide as a malaria control strategy.
Tabitha Mwangi, Researcher, Senior Lecturer, Pwani University
This article was originally published on The Conversation. Read the original article.