Given the fact that there are seven billion people on Earth, one might conclude that human beings are pretty good at reproducing. But fewer than 30% of all fertilization events result in successful pregnancy, even for young, fertile couples.
The remaining 70% of conceptions result in pregnancy loss, with most of these losses occurring before the mother misses a menstrual period. This means that many pregnancies begin and end before the mother even notices. These early pregnancy losses are one reason why it generally takes several months for couples to achieve a successful pregnancy. But why is pregnancy loss so common?

Larsen et al. BMC Medicine 2013 11:154
Current evidence suggests that both the process of egg formation (this is called meiosis) in the mother’s ovaries and the initial embryonic cell divisions (called mitosis) just after fertilization are extremely error-prone, producing embryos with too many or too few chromosomes.
What happens after fertilization?
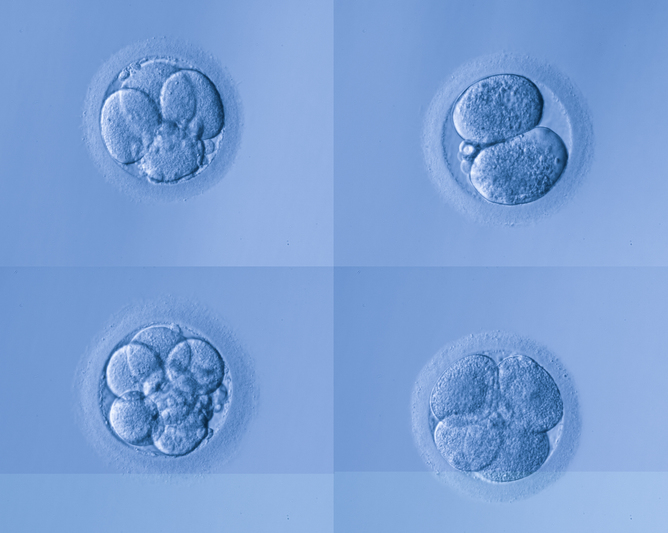
During fertilization, the sperm and egg fuse so that the resulting embryo will have 23 chromosomes inherited from the father and 23 chromosomes inherited from the mother. If all goes well, the subsequent cell divisions in the embryo (called mitotic divisions) simply replicate this 46-chromosome set as new cells are formed.

Stefano Santaguida and Angelika Amon, MIT
Chromosomes contain genes, the blueprints for human development. When processes go awry in meiosis or mitosis, chromosomes can go into the wrong cell or get lost completely, drastically altering this blueprint. The resulting cell will not possess the standard 46-chromosome set – an imbalance that is the defining feature of aneuploidy. This means that many genes will either be missing or present in extra copies, placing cells under stress.
Embryos with many aneuploid cells rarely survive. Trisomy 21, the genetic cause of Down syndrome, is one of the rare forms of aneuploidy in which the baby can survive to live birth. The vast majority of embryos affected with other aneuploidies perish in early development.
What causes aneuploidy?
Aneuploidy is associated with maternal age. Female meiotic errors (these are errors in the eggs themselves) increase from a frequency of less than 20% in mothers younger than 30 years old to greater than 60% in mothers older than 45. Errors in sperm, called paternal meiotic errors, are comparatively rare, affecting fewer than 5% of sperm cells.
But age isn’t the only factor influencing aneuploidy. Our recent work in collaboration with the genetic testing company Natera, published in Science, suggests that risk is also influenced by a common genetic variant in the mother’s genome.

Henry Vandyke Carter via Wikimedia Commons
Even when the egg and sperm are normal, aneuploidies often arise after fertilization, during the first three embryonic cell divisions. These initial cell divisions of the embryo are controlled by maternal machinery pre-loaded into the egg.
Unlike meiotic errors in the egg, mitotic errors do not increase with age, but affect all age groups.
A maternal genetic variant influences aneuploidy risk
Using data from in vitro fertilized (IVF) embryos screened by our collaborators at Natera, we found that mothers with a particular genetic variant on chromosome 4 tend to produce embryos with more mitotic aneuploidies – the aneuploidies that arise during post-fertilization cell division.
This effect was observed for mothers of all ages and from diverse ethnic backgrounds. This genetic variant is surprisingly common; approximately half of all people carry at least one copy of this risk variant.
The most likely suspect is a gene called Polo-like kinase 4 (PLK4), which is known to be a master regulator of the centrosome cycle. The centrosome is molecular machine that is responsible for proper cell division and distribution of chromosomes.
We estimated that each copy of the risk variant increases the rate of aneuploidy by about 3%, regardless of the mother’s age. Having two copies doubles this risk. This increased risk could be especially important for older mothers who are already more prone to aneuploidy. It is likely that there are other genetic variants that contribute to aneuploidy risk to a lesser degree, and further work will be required to determine if this is the case.
Because of the established link between aneuploidy and pregnancy loss, we hypothesized that the aneuploidy risk variant might also affect embryo survival. We found that mothers with the high-risk genotypes had fewer embryos available for testing, suggesting that their embryos are less likely to survive very early developmental stages due to aneuploidy.
Given these results, it seems like this genetic variant could influence the average time it takes to achieve successful pregnancy, an idea that we are hoping to investigate further.
A signature of natural selection: comparison to the Neanderthals
Normally, natural selection weeds out damaging variation, reducing it to very low frequency. But the aneuploidy risk variant is very common. Hoping to learn more about the evolutionary history of this variant, we compared human genomes to Neanderthals and Denisovans, our ancient hominin relatives.

hairymuseummatt (original photo), DrMikeBaxter (derivative work) via Wikimedia Commons, CC BY
Despite the fact that the harmful genetic variant is relatively common in humans, it was absent in these close relatives, meaning that it likely rose rapidly in frequency in an ancestral population of humans. If this is true, it means that this version of this gene was actually somehow beneficial (and maybe still is) while simultaneously being harmful in the context of early development.
So what could possibly have been the benefit?
We aren’t sure at this point, but we speculate that for ancient humans, there might have been a benefit to having a reduced probability of successful pregnancy per intercourse. Maybe the benefit had to do with infanticide – men may be less likely to kill a baby if there is a chance it is their child, and not that of a rival. Likewise, lower probability of pregnancy per intercourse might encourage repeated mating with the same female, fostering pair bonding and paternal investment. This hypothesis was first proposed by Alexander and Noonan in 1979 to help explain the human-specific trait of concealed ovulation and continuous sexual receptivity – women do not externally signal or limit intercourse to the fertile portion of their cycles as do some other primates.
Another idea is based on the fact that PLK4 is often mutated in human cancers. Could there be a beneficial effect of the risk variant in the context of cancer? PLK4 plays yet another role in testes development. Could the aneuploidy risk variant have a beneficial effect in this context?
We are hoping that additional data and future research can shed more light on this signal of human-specific adaptation. Is it real or simply an artifact of chance events in human evolution? Did our ancestors have lower rates of aneuploidy? What about Neanderthals, Denisovans, and living non-human primates? And perhaps the most basic question: why is human aneuploidy so common? Armed with modern genomic technologies, we can continue to chip away at these questions to understand not only the medical aspects of aneuploidy risk, but also the broader evolutionary basis of this intriguing trait.
![]()
This article was originally published on The Conversation.
Read the original article.