Jeremiah Waweru Gathirwa, Kenya Medical Research Institute and Ruth Monyenye Nyang’acha,, Kenya Medical Research Institute
It will take effective prevention, accurate and timely diagnosis and treatment to successfully eliminate malaria. But none of this will help if the causative agents become resistant to the drugs used for treatment. The Conversation Africa’s Health and Medicine Editor Joy Wanja Muraya spoke to Dr. Jeremiah Waweru Gathirwa and Ruth Monyenye Nyang’acha researchers at the Kenya Medical Research Institute about the country’s work towards using medicinal plants as a potential anti-malarial drugs. ![]()
What is the place of medicinal plants in Africa generally and in Kenya more particularly?
Most communities heavily rely on medicinal plants to prevent and treat diseases. About 80% of people in Africa depend on traditional medicine. Traditional healers prescribe medicinal plants to treat various illnesses. These plants are an accessible and affordable form of treatment for communities across the continent.
Medicinal plants have ingredients that can treat a condition or disease or can be used to manufacture useful drugs.
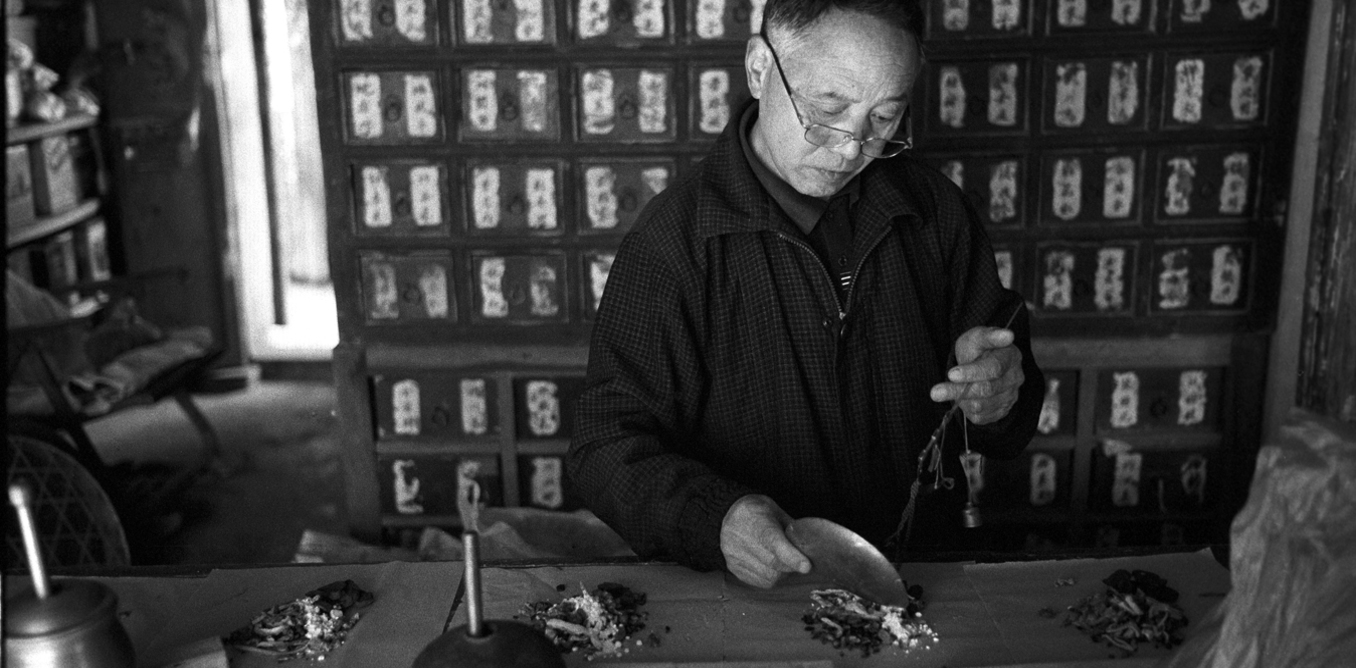
Herbal medicines are an important part of culture and traditions all over the continent and beyond. For centuries people have used their knowledge about the environment to treat various ailments. For example, the Chinese herbalists have used extracts of the Qinghao plant; Artemisia annua also known as sweet wormwood for malaria treatment for over 1,500 years.
The old-age use of herbal medicines is true of several communities in Kenya – where malaria is among the ailments they’ve treated.
Why is it important to consider medicinal plants as potential sources of anti-malarial drugs?
Malaria is preventable and treatable. But it’s a major public health problem in Kenya: there are an estimated 6.7 million new cases and 4,000 deaths each year.
It accounts for 15% of all out patient attendance in Kenya’s health facilities’ admissions.
Drug resistance has led to most of the malaria drugs in the market becoming ineffective in treating the disease. There is therefore an urgent and continuous call to search for new antimalarial agents.
Most of the drugs used to treat malaria are either derived from plants or are products of natural sources.
For example quinine, an antimalarial, comes from the medicinal plant Cinchona succirubra. Artemisinin is derived from Artemisia annua, another medicinal plant. These previous successes underscores the importance of medicinal plants in the fight against malaria and as a rich reservoir from which new antimalarial drugs can be developed.
Scientific evaluation for safety, efficacy and quality of medicinal plant preparations is important in safeguarding users. From our research, we found out that that medicinal plants are a potential source of new antimalarial drugs or preparations.
What did the study set to achieve? What were the findings?
The aim of the study was to identify and evaluate the safety of sampled medicinal plants in treating malaria. We selected 48 plants through interviews with traditional healers from malaria endemic zones in Kenya. The areas included Siaya in western Kenya, Mwea in Central Kenya and regions in the coastal belt.
These plants have historically been used by traditional health practitioners to treat malaria and we subjected them to laboratory tests in search of their anti parasitic properties.
We also investigated whether the plants were used singly or in combination with others. After testing all the selected plants for their antimalarial efficacy, we found the following six plant species to have the highest potential.
*Azadirachta indica
*Fagaropsis angolensis
*Rhus natalensis
*Zanthoxylum usambarense
*Cissampelos pareira
*Grewia plagiophylla
These medicinal plants depicted the highest ability to kill the malaria parasite.
We tested the effect of combining some plant extracts against a multi-drug resistant malaria parasite, Plasmodium falciparum and observed that in some cases the plants depicted higher efficacy when in combination as opposed to the single extracts.
Some of the tested plants showed mild toxicity against cultured mammalian cells. This is a test that involves growing human cells in the laboratory and exposing them to the plant extracts to test whether the extracts will have a negative effect to the growth of the cells as an indication of poisonous effect. All the other tested plant extracts were found to be safe.
The safety results of the medicinal plants were impressive because they showed that they were able to select the malaria parasites and effectively kill them.
What’s promising about your research?
The study identified plants that have medicinal qualities that kill the malaria causing parasite. Our study also confirmed that combining some medicinal plants with other species, as is done in traditional medicine, works.
The preliminary results showed that there’s great potential of developing safe and efficacious antimalarial medicines from the natural extract of local plants.
Adopting medicinal plants as sources of antimalarial treatment will be beneficial for Kenya because the drugs would be cheaper to produce, more cost effective for patients and easily accessible.
What are the next steps to making this a reality?
Kenya Medical Research Institute is working to develop a safe and effective antimalarial drug based on these natural products. We are working to establish appropriate dosages and mode of administration for effective treatment in humans. This is guided by reports from the laboratory and animal experiments.
A well conducted clinical trial of the best performing antimalarial preparations will be conducted prior to advocating the same for clinical application in primary health care.
We are also working with communities where these high value medicinal plants are found so as to encourage their preservation as sources of raw materials for the preparation of antimalarial medicines. We also hope to begin cultivating these plants as a future source of the raw material and as an income generating activity for the engaged communities.
Jeremiah Waweru Gathirwa, Researcher in Chemical Biology, Biochemistry, and Medicinal Chemistry, Kenya Medical Research Institute and Ruth Monyenye Nyang’acha,, Medical Parasitologist, Research Officer,, Kenya Medical Research Institute
This article was originally published on The Conversation. Read the original article.