OF MICE AND DIRT
At this very moment, there is a mouse who although appears a bit dogged and raggedy is actually quite animated and bears a wild spirit as he sniffs, scrambles, and snoops about his cage at the University of Texas Health Science Center at San Antonio. Though next to his younger siblings he appears on the runtier end of the litter, unlike them he boasts a coat of black fur lustrous enough to land him a spot on a Pantene commercial. Our said mouse’s name is Mouse UT2598 and he is 3 years old, which translates into the centennial years when it comes to a human life span, as mice typically live to around 4 years old, if they are lucky.
For the sake of this article, let’s call this mouse Mighty. So, what gives Mighty his punk-ass edge? It’s called rapamycin, a compound which is gradually revealing to scientists its ability to slow the aging process along with the havoc it can cause on certain cells. Mighty’s heart and liver are functioning as if he were an adolescent, and his tendons are far more resilient with the elasticity of a 3 year-old mouse. Evidence also reveals that his organs are damaged markedly less than is considered standard at his age, leading to the theory that Mighty may be spared the effects of cancer for quite some time longer than mice not involved in the experiments taking place at the University of Texas. In fact, place him in a line-up alongside other mice his age and the distinctions are absolutely extraordinary.
The experiment involving Mighty and rapamycin is just one of many when it comes to investigation into the aging process. Research all over the globe entails experiments with a plethora of agents, not just rapamycin, some of which are already being used to treat a number of human conditions. Scientists are assembling the puzzle by employing tactics like manipulating genes, too. Essentially, they are all in a race for the big cheese: finding ways to extend longevity and ultimately trap the aging process and curb – if not cure (or even reverse) – it altogether.
As it stands, aging is the single most potent ingredient when it comes to recipes needed for age-related diseases that eventually shorten our lives like cancer, heart conditions, Alzheimer’s and other degenerative brain ailments, and others. While the main components typically associated with heart disease are high cholesterol, obesity and high blood pressure, simply celebrating an 80th birthday can be the factor that tips the scale towards contracting a fatal heart condition – even if that 80 year-old resisted a single nibble of his birthday cake. That being said, scientists are beginning to treat aging as a disease in and of itself, one which may be sensitive to treatment as simple as a doctor’s prescription.
Let’s get back to Mighty and his happy pill. Rapamycin has its origin in dirt. That is, soil samples which were collected in 1964 on a voyage to Easter Island eventually became the foundation for developing the antibiotic, and researchers have found that mice who were given the drug were prone to longer lives (about 20% longer) than mice who did not ingest the medication. What makes rapamycin particularly interesting is that it functions in a variety of species including yeast, worms and flies – and it works even when started late in life. Thus, if studies involving the drug are successful and actually lead to human treatment, it could potentially offer benefits to those starting it in their 60s or even 80s.
HOW DOES RAPAMYCIN WORK?
Rapamycin essentially hinders the operation of a gene that both people and mice possess. It is a gene called mTOR which gives the “Okay To Go” to cells for absorbing and expending energy. In the case that there is an abundance of cell-chow, mTOR gets busy directing cells to take in nutrients and start growing. When food is in short supply, the gene retracts as a turtle would into its shell until the next opportunity to feast arises. Scientists have discovered that when cells are active and “eating”, they age substantially, chiefly due to the fact that they are working their cell-butts off to process food while belching out toxic free radicals at the same time. Thus, the mission is to metaphorically slip that cell a “mickey” and keep it mellowed out without putting it at risk of starving itself – and that’s just what rapamycin is allegedly capable of doing. But – and there’s always a but when it comes to this sort of thing – rapamycin is far from being the long-searched-for fountain of youth. In studies like that starring our friend Mighty, rapamycin has resulted in a body that is 30% smaller than average while mTor-manipulated mice developed cataracts and proved more susceptible to diabetes. The study also showed that males are inclined to progressively lose testicular functioning – not exactly a perk when it comes to a pill that may help you live longer.
Another disadvantage of rapamycin was revealed when humans who were administered the drug after kidney transplants in order to decrease the risk of rejection showed signs of higher susceptibility to diabetes. Despite this, scientists feel positive when it comes to their abilities to whip up a tantalizing cocktail when it comes to adjusting doses and arriving at the ideal blend to increase the pros when it comes to longevity rather than the cons of any possible risks.
GENETIC SOLUTIONS – AND COMPLICATIONS
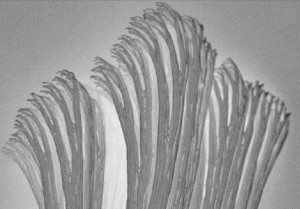
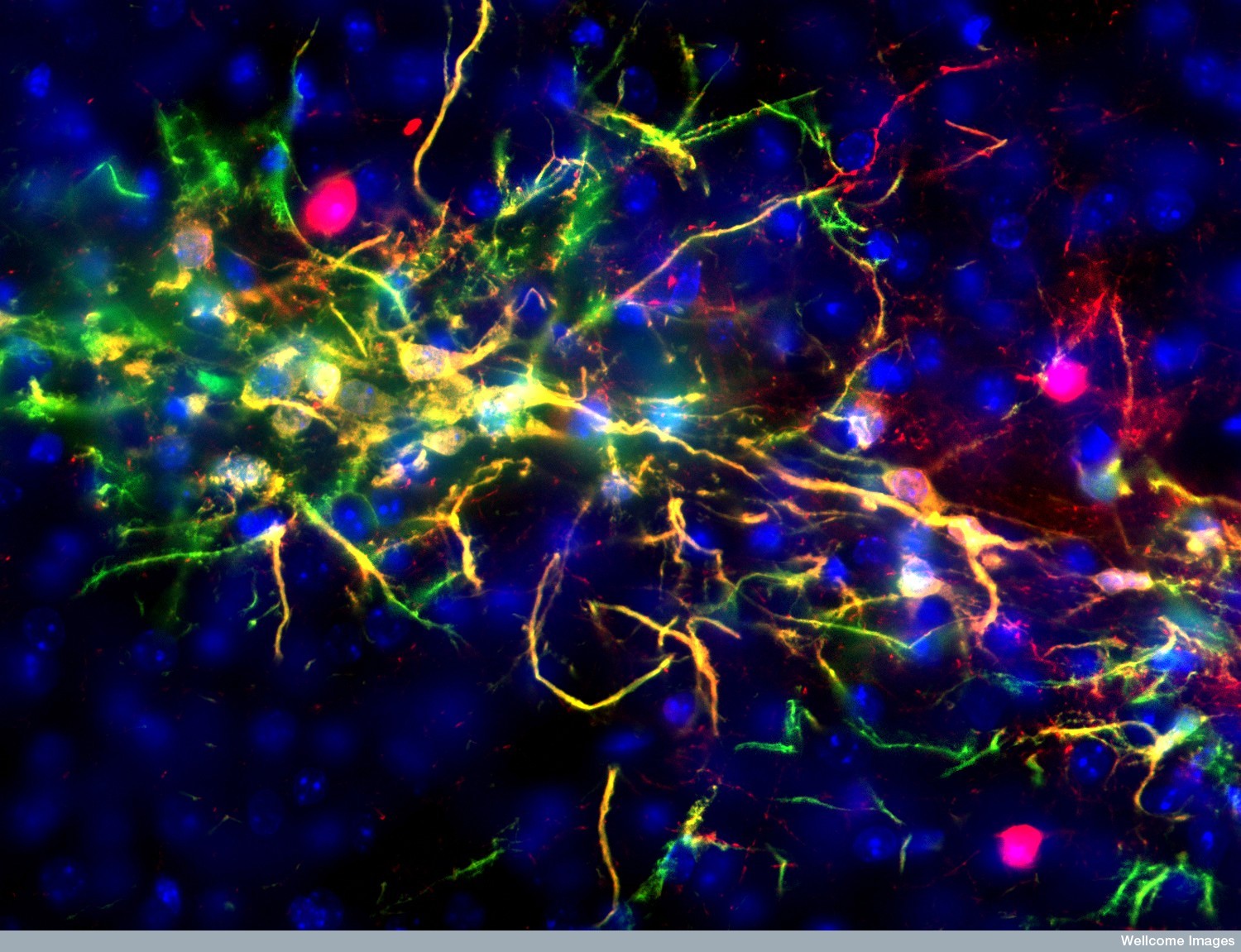
For some researchers, the passcode for achieving longevity lies in our genes, particularly when it comes to telomeres which are essentially timekeepers of a cell’s life. When a cell divides, it automatically xeroxes its chromosomes’ DNA and telomeres carry the responsibility of cueing when to halt that copying process. Every cell division triggers squiggles of DNA to essentially tie themselves into a knot at the end of a thread (or chromosome) and eventually vanish for good. Certain factors can cause telomeres to shorten cell lives at different rates (like exposure to UV light), making them a perfect target for further research regarding the scavenger hunt for anti-aging formulas.
Healthy human bodies typically maintain a perfect waltz between telomeres and telomerase (an enzyme that handles the lengthening or shortening of DNA strands) so that telomerase can lengthens telomeres just enough that an ideal amount of lost DNA can be retrieved back. But in individuals with telomere-syndrome, ailments like bone problems, liver failure and immune disorders can occur. Discovering how to tame malfunctioning telomeres can lead to correcting their misbehavior and coming up with aging-combatant formulas.
Just over a decade ago, a scientist and her collaborator, Dr. Mary Armanios and Carol Greider (the co-discoverer of telomerase) respectively, worked together in a lab at Johns Hopkins University and met a student with a blood disorder that necessitated blood transfusions on the regular. The boy was in his 20s and already had a full head of startlingly gray hair, signs of which began showing when he was only 9 years old. Curiouser and curiouser, Armanios and Greider learned that all of his paternal relatives had died at staggeringly young ages including his grandmother who died of osteoporosis in her 60s, his father who died at 59 while waiting for a liver transplant, and his aunt and uncle who both died of pneumonia in their 60s. What’s more, the boy himself had suffered from various infections that landed him in the hospital multiple times a year – and he eventually died of a staph infection at 31. It turned out that all of the family members had a severe form of telomere malfunction known as dyskeratosis congenita.
To date, Armanio feels strongly that she will learn a lot by tinkering with telomeres, including how they can be engineered to halt aging-related ailments. Similar interest lingers at Stanford University where Helen Blau and her co-researchers have splashed cells with the precise amount of genetic matter to encourage the lengthening of telomeres. In her study, cells ceased to divide indefinitely and on the contrary started to deteriorate at a normal pace, sparking hope in Blau and her team that the cells might be used for testing in the bodies of people with dyskeratosis congenita. If the cells can target the abnormally rapid growing cells entailed in the disease, they might also be used to create techniques for turning back time on normal human aging cells.
SIAMESE-MICE (YES, YOU READ THAT CORRECTLY)
There exists promises of age-defiance in another quite odd experiment taking place at the Harvard Stem Cell Institute. There, researchers have pinned their hopes on the cousins of our friend Mighty – but in a very unusual way. To conduct their work, scientists conjoin two mice, Siamese-twin style, so that they share the same blood system. Via this most bizarre procedure, it’s been discovered that among of a pair of harnessed mice, the older one presents more new nerve-cell growth in their brains than the younger one. The elders were also brawnier, and boasted a reversal of the heart-enlargening process that typically goes hand-in-hand with aging.
The mysterious component that appears to be the cause of these findings is a protein called GD11 which is normally aplenty in young animal blood and meager in older blood. Naturally, the team at Stanford is clawing away at this amazing discovery in hopes of unearthing an answer to the question of whether or not people who live longer have higher levels of GD11, or whether people with little amounts of the protein prove more liable to develop age-related diseases like heart complication, muscle atrophy and cognitive deterioration.
DOES LONGEVITY HAVE ITS ROOTS TO GREEK MYTH?
At the University of California, San Francisco, another experiment is taking place under the auspices of neurobiologist Dena Dubai and involves a hormone called called klotho. Klotho received its nomenclature after the Greek fate responsible for spinning the thread of life for mortals. Klotho is known for extending the lives of animals by 30% when in increased levels. Approximately 1 in 5 humans carry enough of the protein to tack on an extra 3 or 4 years to their lives and although it is not a passport to the land of immortality, it is certainly a bigfoot-sized step towards that mystical destination.
MORE BIRTHDAYS ON THE HORIZON
On that note, it is important to keep in mind that most – if not all – research is not fixed on the objective of creating neverending lifetimes, rather extending healthy lives a bit longer. While toying around with components like telomeres, klotho, and GD11 offer promising results, it is not as easy as simply whipping up the perfect recipe and stocking up Rite-Aid shelves. Further manipulation of longevity genes could involve some big league moves like gene therapy and cell transplants and of course first solving all of the questions that pop up with each answer a scientist reaches. While these riddles are the culprit for bringing researchers back to the drawing board again and again, the general outlook for battling the effects of aging is remarkably upbeat. Scientists seem to bear a spirited momentum certain to bring about some serious headway in the not-too-distant future.